Animal cells share some qualities with plant cells, but one key feature ours lack is a rigid cell wall. While this provides structure for plants, it’s also something scientists are increasingly looking at for use in new materials, cellulose technology and, now, insulin delivery.
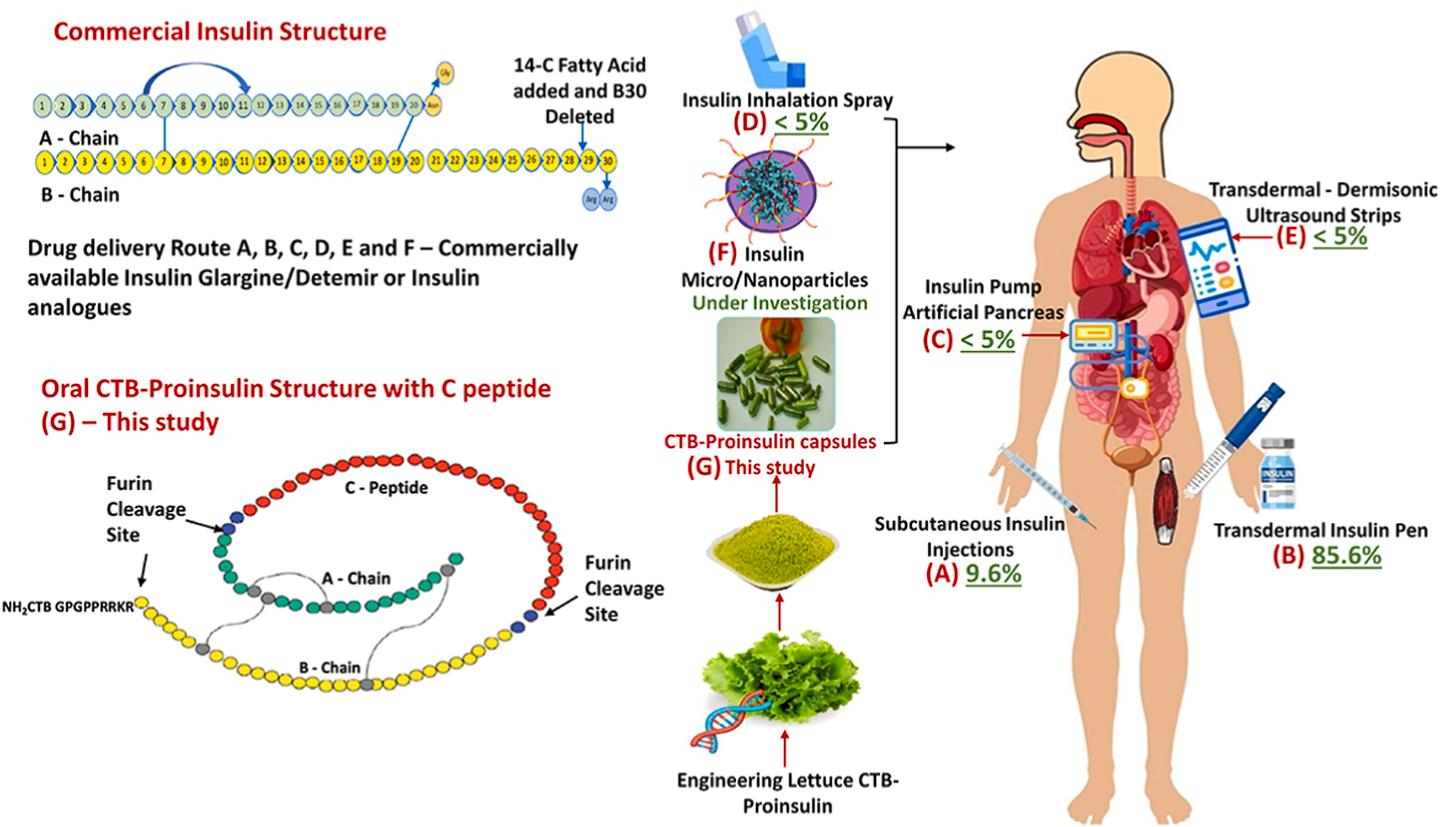
Led by Henry Daniell from the University of Pennsylvania’s School of Dental Medicine, researchers have created a promising plant-based insulin, containing the three peptides that occur naturally in insulin, which can also be ingested orally.
Just as important as the genetic material on the inside, the plant cell walls are key to the drug’s efficacy. Their sturdiness shields the insulin from upper digestive tract acids and enzymes, until the drug reaches the microbes in the gut, which work to release the insulin. From here, the insulin travels via the gut-liver axis to reach its destination.
In the trial on mice, the plant-based insulin was able to regulate blood sugar within 15 minutes, comparable to naturally secreted insulin. Mice treated with traditional insulin injections experienced crashing blood glucose levels leading to hypoglycemia.
“The risk of hypoglycemia is one of the biggest disadvantages of the current delivery system and can even result in a coma,” Daniell said. “Our insulin, given orally, has all three proteins and is delivered right to the liver. It works just like natural insulin, which minimizes the risk of hypoglycemia.”
Current medications such as injections via insulin pen run the risk of hypoglycemia, while the precise medicine delivery offered by an insulin pump requires prohibitively expensive hardware. Current machinery costs around US$6,500 and has a lifespan of three to four years.
As for the medicine itself, a complex process of genetic engineering essentially sees a “gene gun” used to blast human insulin genes through the plant cell walls. These genes become incorporated into the plant’s genome, and over generations will be selectively bred from seeds that retain the blueprint, to have all grown plants capable to be used for their insulin.
The research found that although this part of the genome changed, there were no adverse effects seen in the plant nor the animals in the trial.
With the genes intact, the lettuce could be freeze dried, ground and prepared for oral delivery.
The teams sees another huge advantage in this approach to insulin. Current clinical production requires growing the hormone in bacteria or yeast cells, under controlled laboratory conditions, storage and transport.
“We’ve seen news stories about vaccine doses being destroyed because some countries don’t have the resources for cold storage throughout the process,” Daniell said. “It is an enormous cost. This kind of post-production cost is eliminated using our methods because we have shown repeatedly that the product is shelf-stable.”
While the results in the mice study are hugely promising, there’s still some time to go before this method could benefit many of the estimated 537 million adults living with diabetes. But the researchers are confident of moving onto a bigger trial, first with diabetic dogs, then humans.
“A lot of dogs have diabetes, and the owners have to be home to give insulin three times a day,” Daniell said. “We’ve done canine studies in the past in dogs with hemophilia or heart disease, and we know how to mix the plant powder in their food and add some bacon flavor. They love it.”
That 2015 study to treat hemophilia with modified lettuce also shows the potential of effective, inexpensive and accessible plant-based therapies for a wide range of conditions.
“With this delivery system, we change the whole paradigm, not only for insulin,” he added. “I grew up in a developing country and saw people die because they couldn’t afford drugs or vaccines. For me, affordability and global access to healthcare are the foundation for my work. And in this case we are making insulin more affordable while significantly improving it. Patients can get a superior drug at a lower cost.”
The study was published in the journal Biomaterials.
Source: University of Pennsylvania
Source of Article